A colposcopy is a simple procedure used to look at the cervix, the lower part of the womb at the top of the vagina. It's often done if cervical screening finds abnormal cells in your cervix.
These cells often go away on their own, but sometimes there's a risk they could eventually turn into cervical cancer if not treated.
A colposcopy can confirm whether cells in your cervix are abnormal and determine whether you need treatment to remove them.
When a colposcopy may be needed
You may be referred for a colposcopy within a few weeks of cervical screening if:
- some of the cells in your screening sample are abnormal
- the nurse or doctor who carried out the screening test thought your cervix did not look as healthy as it should
- it was not possible to give you a clear result after several screening tests
A colposcopy can also be used to find out the cause of problems such as unusual vaginal bleeding (for example, bleeding after sex).
Try not to worry if you've been referred for a colposcopy. It's very unlikely you have cancer and any abnormal cells will not get worse while you're waiting for your appointment.
What happens during a colposcopy
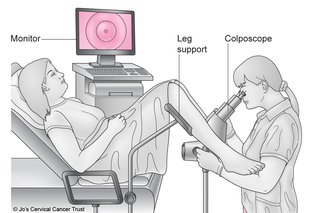
A colposcopy is usually carried out in a hospital clinic. It takes about 15 to 20 minutes and you can go home the same day.
During the procedure:
- you undress from the waist down (a loose skirt may not need to be removed) and lie down in a chair with padded supports for your legs
- a device called a speculum is inserted into your vagina and gently opened
- a microscope with a light is used to look at your cervix – this does not touch or enter your body
- liquids are applied to your cervix to highlight any abnormal areas
- a small sample of tissue (a biopsy) may be removed for closer examination in a laboratory – this may be a bit uncomfortable
If it's obvious that you have abnormal cells in your cervix, you may have treatment to remove the cells immediately. If this is not clear, you'll need to wait until you get your biopsy results.
Read more about what happens before, during and after a colposcopy.
Results of a colposcopy
It's often possible to tell you right away if there are any abnormal cells in your cervix. But if you had a biopsy, it may take 4 to 8 weeks to get your results in the post.
The result of your colposcopy and/or biopsy will be either:
- normal – about 4 out of 10 people have no abnormal cells and are advised to continue attending cervical screening as usual
- abnormal – about 6 out of 10 people have abnormal cells in their cervix and may need treatment to remove them
Your doctor or nurse may use the term CIN or CGIN when discussing your biopsy result. This is this medical name for abnormal cells.
It's followed by a number (for example, CIN 1) that shows the chances of the cells becoming cancerous. A higher number means a higher risk of cancer developing if the cells are not removed.
Read more about colposcopy results.
Treatments to remove abnormal cells
Treatment to remove abnormal cells is recommended if there's a moderate or high chance of the cells becoming cancerous if left untreated.
There are several simple and effective treatments that can be used to remove the abnormal cells, including:
- large loop excision of the transformation zone (LLETZ) – a heated wire loop is used to remove the abnormal cells
- a cone biopsy – a cone-shaped piece of tissue containing the abnormal cells is cut out from your cervix
LLETZ is usually carried out while you're awake but your cervix is numbed. You can go home the same day.
A cone biopsy is usually done under general anaesthetic (where you're asleep) and you may need to stay in hospital overnight.
Read more about colposcopy treatments.
Page last reviewed: 30 December 2019
Next review due: 30 December 2022